business

Illustration by Jon Krause / www.jonkrause.com
Policing medical practice employees after work
■ Doctors can try to regulate staff actions outside the office, but they must watch what they try to stamp out and how they do it.
The University of Pennsylvania Health System and its affiliates recently joined Cleveland Clinic and other hospitals in banning the employment of smokers. Proponents say such policies lower health care costs and improve employee and community health. Others believe these restrictions may be the beginning of a slippery ethical slope in which employees can be fired or banned for personal decisions and activities unrelated to their specific jobs.
The question is: Will and can private physician practices soon follow suit, banning or disciplining employees not only for smoking but also for other outside activities deemed detrimental to the image of the group? What about obesity, social media presence, hobbies and other after-work activities? Are there legitimate situations where the needs and mission of the practice, and the protection of its patients, outweigh the individual rights of the employee and potential employee? In general, are these types of bans legal and ethical?
These issues, say human resources, health policy and legal experts, are complex and evolving.
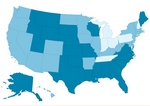
The University of Pennsylvania Health System and Cleveland Clinic can ban smokers because Pennsylvania and Ohio are not among the 29 U.S. states that prohibit smoker hiring bans.
“Generally speaking, if you want to regulate off-duty conduct, your starting point should be a review of the governing state law, as different states have different laws,” said Lori Rassas, employment attorney and author of Employment Law: A Guide to Hiring, Managing and Firing for Employers and Employees.
“Some states specifically protect legal products; others, legal conduct,” she said. “If there is no state law [specifically pertaining to the behavior], then employers should be prepared to explain the nature of its legitimate business interest that would justify this intrusion. Employers are most successful at regulating the off-duty conduct of its employees if the conduct is related to activity that directly impacts the employee's ability to do [his or her] job.
“Courts are increasingly reluctant to allow employer intrusiveness; they really look to the underlying reasons why the employer believes the regulation is necessary for the employer to run its operations.”
The idea of banning employment or terminating an employee because of their after-hours activities is problematic, said Michael Siegel, MD, professor of community health services at the Boston University School of Public Health.
“I'm making an ethical argument,” he said. “The first thing is that not hiring smokers is employment discrimination. People who support these policies are basically saying that they are OK with employment discrimination under certain circumstances. You quickly realize how dangerous that is.”
When pertaining to employee health habits, the situations “are identical whether it's a large hospital or a private practice,” Dr. Siegel said. “Health care expenditures are important. The benefits are similar; the drawbacks are the same. It's still discrimination. My guess is that [these types of bans] are gaining steam.”
While banning smoker employment is not illegal in some states, Philip Dickey, human resources services director/partner of Doctors Management Inc. in Knoxville, Tenn., said he is seeing a trend. Practices “are identifying themselves, if allowed, as nonsmoking facilities on the [employment] application and in the interview.
DID YOU KNOW:
29 states prohibit hiring bans against smokers.
“I advise physicians to tell potential employees during the interview: 'We are a nonsmoking practice. Are you comfortable with that?' I would not suggest asking a person directly: 'Do you smoke?' ”
Enforcing wellness
Obesity is another issue that can affect a practice's bottom line, as individuals who are overweight or obese are more likely to have co-morbidities that are costly to insure and treat. A practice striving to promote healthy patient habits may feel that staff should reflect the practice mission.
“There is no question that there are data that show that people who are overweight cost a lot more money,” Dr. Siegel said. “An employer could say, 'We are going to have a BMI [body mass index] limit. If it's over a certain number, you're not going to be hired.' Like smoking, such requirements could save in health care costs and help boost the overall health of the employee population.” However, Dr. Siegel said, “once you open the door and say employment discrimination is OK, pretty much any employment discrimination” becomes possible.
“Obesity in and of itself is not a protected class,” Dickey said. But many diseases and conditions caused by or related to obesity can be protected under regulations of the Americans with Disabilities Act.
“What's important is that when you try to hire people that you hire them for their skill set,” Dickey said. “What I tell my clients is that it's in the best interest of the practice to give everyone a fair shot. If they're the best candidate, select them. Don't not select them because they are obese.”
Once an employee is hired, can you force him or her to modify behaviors, such as smoking and overeating?
“A doctor may want to say to an obese employee or an employee who smokes, 'I want you to exercise and eat healthy, or I want you to stop smoking or you can't work here anymore,' ” Rassas said. “In the absence of state or federal law regulating this condition, the courts will apply a balancing test to determine whether there is something about the employee's obesity or smoking that would prevent them from doing their job. It's a pretty high burden.”
More recently, office- and company-sponsored wellness programs have faced greater scrutiny.
“The general rule is that these programs have to be voluntary,” Rassas said. However, “there is an ongoing debate over how to define 'voluntary.' If you offer incentives for employees to attend a wellness program, such as a gift card or other bonus, then is it an indirect penalty for those who choose not to participate?” Employers must remember that information gathered in a wellness program must remain confidential and off-limits to supervisors and employers. For example, the Genetic Information Nondiscrimination Act prohibits employers from collecting genetic information or family medical history related to their employees.
Regulating Facebook and Twitter
When it comes to social media, employees “enjoy expansive rights … to discuss terms and conditions of employment with other employees,” Rassas said. These rights emanate from the National Labor Relations Act, which applies to both union and nonunion employees in the U.S.
However, if the communication is not “for the mutual aid and protection of fellow employees” or related to a legitimate work issue, “employers need to step back, take a deep breath and look at it very clearly,” Dickey said.
A slanderous posting may be grounds for termination. The challenge is that these issues “are not always black and white. That's what can keep people scratching their heads,” Dickey said.
Violating the Health Insurance Portability and Accountability Act could be grounds for action.
“For example, if it is determined that an employee's distribution of patient photographs via social media violates HIPPA, then it could likely be used as the basis for the imposition of discipline or termination, even if the distribution occurred off-duty, because the employer could argue that misconduct relates to the core” business of the physician practice, Rassas said.
Finally, employees observed engaging in after-work activities deemed potentially embarrassing or unethical, while raising the ire of practice employees, can be a gray area that requires tremendous caution.
“At times you hear of physicians or employees who see a co-worker frequenting a bar or doing something that they don't approve of in their night life, and they're afraid that it might hurt the reputation of the practice,” Dickey said. “That's a legitimate concern to a degree.” However, “you have to be careful that you don't discipline or terminate someone for something that is private. First of all, what you're thinking may be all speculation, and may not be true or real. It's important for employers to step back [and ask themselves], 'Is this really hurting us? Can we prove this? Or are we just speculating that it could?' ”
But if the employee's off-duty conduct prevents that person from doing his or her job, “then the employer would likely have the right to regulate it,” Rassas said.
For example, if a nurse practitioner engages in off-duty conduct that results in the loss of the license that enables him or her to prescribe medication, an essential job responsibility, then the employer probably can use this conduct as the basis for discipline, Rassas said. The activity occurred after work hours, but the consequences have affected the employee's ability to do their job.
“In general, employers need … to take the emotion out of it, look at the facts and take their time,” Dickey said. “Once you pull the trigger [with discipline or termination], it's done.”